This document is a summarised version of Emergency Department DG-CC2-Streaming of Patients at Sunshine Emergency Department. The summary has been created to be Emergency Department specific, and has been endorsed by the SHED Leadership Team. Staff should review the PPG if they require further information.
Overview:
This QRG provides an overview of the streaming model within the Emergency Department (ED). Streaming leads to safe management, timely care provision and improves efficiency within the ED.
Applicability:
This QRG is applicable to all clinical and support staff working within the SHED.
Responsibility:
The SHED Nursing Education Team, Nurse Unit Managers and Adult & Paediatric Directors of Emergency Medicine are responsible for introducing and implementing the streaming procedure.
Guideline/Process Details:
What is streaming?
All patients who present to the SHED are triaged on arrival to rapidly determine acuity and care needs. Following triage, patients are streamed into designated clinical areas of the ED (Pods). Streaming recognises individual patient care needs, selecting the most appropriate team to deliver the right care at the right time.
Who can make a streaming decision?
- ED Nurse in Charge (NIC) of the shift
|
|
- Senior Clinician/Pod Leader (Medical or Nursing)
|
|
- Emergency Mental Health Clinician
|
|
- Mental Health Nurse Navigator
|
|
Streaming points
Patients are streamed at the following points of care within the ED:
- Triage – walk-in or Emergency Services arrival
- Primary screening for acuity, need for rapid assessment and Pod allocation
- Note presentations with pre-defined pathways including stroke, STEMI, Section 351, high acuity pre-notified patients (BAT call), SEPSIS pathway, direct inpatient admission and women presenting with gynaecological or pregnancy complaints
- Streaming guidance for MHAOD presentations also exists (see Appendix A)
- Assessment areas
- Secondary screening in the Triage Assessment Room (TAR), AV Corridor or Behaviour Assessment Room (BAR) to ascertain infectious risk, clinical risk and OVA/safety profile
- SHED cubicle
- Patients may be referred to another Pod as their clinical requirements change
Clinical Pods for streaming
Patients may be streamed to one of the following clinical areas (Pods):
|
|
|
|
|
|
|
|
- Behavioural Assessment Unit (BAU)
|
|
|
|
Each Pod functions independently and contains its own specialised multi-disciplinary team. There are specific criteria for entering each Pod. These criteria, including presentations and procedures, are detailed in the Streaming of Patients at Sunshine Emergency Department Procedure.
Designated MHAOD Accommodations
BAU and The Hub will provide care for all patients between the ages of 18 – 64 years of age who present to SHED with mental health and/or AOD care needs.
- Admission to BAU or The Hub might occur post initial arrival to the department, after an individual has received acute care for their physical health.
- In some instances, patients may need to wait for admission to a point of care. In these cases, the initial assessment and intake will focus on reducing the risk associated with the wait.
Exemptions to BAU and The Hub age criteria can be approved by an ED consultant, or the Senior Medical Officer in Charge (SMOIC). If an exemption does not apply:
- Patients under 18 will be admitted to Children’s Area where, if required, children can receive MHAOD care upon referral to EMH and ED AOD services.
- EMH and ED AOD clinicians will review or provide consultation to patients 65 and older when they have been admitted to general ED cubicles/Adult Acute Area, or Resus Area as clinically indicated.
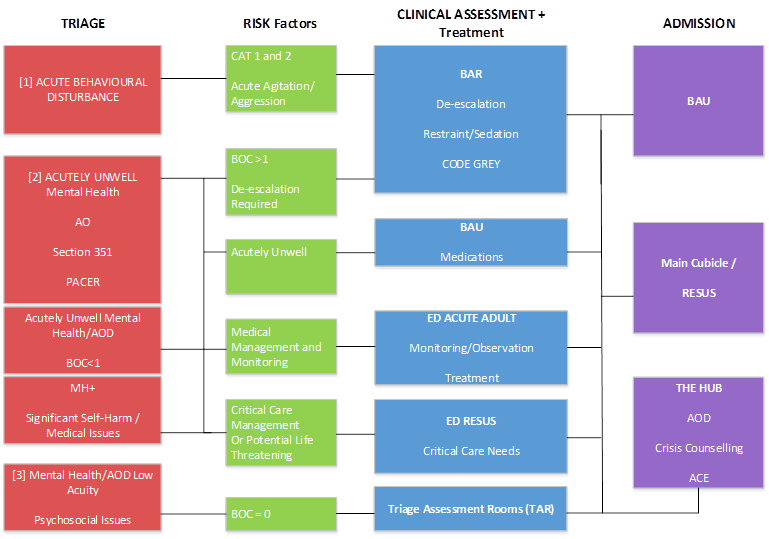
MHAOD Streaming Guidance
While patient streaming decisions are led by clinician decision making and real-time assessment of the situation, high-level patient streaming guidance for patients 18 to 64 with mental health and AOD care needs is outlined in Appendix A. This diagram indicates appropriate streaming pathways for the following presentations:
[1] Patients presenting with acute behavioural disturbance:
Facilitate de-escalation via a planned code grey and transfer to a BAR (LOS <=30 minutes).
Subsequent patient admission is based on clinician assessment, including response to de-escalation and/or need for restraint/sedation.
Examples of subsequent admission:
| Patients with ongoing acute agitation or aggression / need for restraint and sedation |
->
|
May be suitable for BAU admission |
| Patients who have responded to de-escalation and still pose an ongoing violence risk, and / or have been assessed as requiring ED medical care |
->
|
May be suitable for an ED cubicle |
| Patients who have been assessed as no longer posing a violence risk, and not requiring ED medical care |
->
|
May be suitable for The Hub admission |
[2] patients presenting in behavioural crisis with MHAOD care needs:
This includes patients arriving under the Mental Health Act 2014 (VIC), patients self-referred or referred by family/carer, and patients presenting with significant self-harm or suicide ideation or behaviour.
| Patients with a BOC score >=1 |
->
|
May require de-escalation intervention that can be facilitated in a BAR |
| Patients who are assessed as acutely unwell owing to AOD issues – including experiencing intoxication or withdrawal that elicits behaviours of concern (BOC) |
->
|
May be admitted to BAU for observation and appropriate medical or pharmacological intervention |
| Patients who are assessed as requiring ED medical care |
->
|
May be admitted to ED Adult Acute |
| Patients who are assessed as requiring urgent/critical care |
-> |
May be admitted to a Resus cubicle |
As before, subsequent patient admission is based on clinician assessment, including response to de-escalation and/or need for restraint/sedation (see previous pathway guidance for examples).
[3] patients presenting with low acuity mental health/AOD issues, or low acuity psychosocial issues:
These are patients who obtain a BOC score of 0, are medically stable and do not present with acute suicide ideation/behaviour.
Transfer to a Triage Assessment Room (TAR) or the BAU Interview Room will facilitate assessment
Patient may be subsequently transferred to BAU, an ED cubicle (including Resus cubicle) or the Hub, based on clinician assessment.
MHAOD Access and Flow
At times the most appropriate point of care may not be available. In this case the Intake and Streaming Team will stream the patient to the next appropriate point of care. The below guidance is given noting it is the clinical decision of the ED Medical Officer/Consultant in-Charge to determine if a treatment space is fit-for-purpose where medical care is required.
Supporting Documentation:
Document Governance
| Title: |
Patient Streaming – SHED |
| Version: |
2.0 |
| Date Published: |
May, 2022 |
| Date of scheduled review: |
May, 2023 |
| Author: |
Approver: |
| SHED Leadership Team |
SHED Leadership Team |