This document is a summarised version of OP-GC2-Pressure Injury Prevention and Management. The summary has been created to combine best practice information into one document specific to the Emergency Department, and has been endorsed by the ED Leadership Team. Staff should review the PPG if they require further information.
Overview
This QRG provides staff with an overview on the Comprehensive patient care involved in the assessment of their skin & risk of pressure injuries on arrival to the Emergency Department.
Applicability
This QRG applies to all presentations to the Emergency Department.
Responsibility
It is the responsibility of the Nurse Unit Managers and Directors of the Emergency Departments of each site to ensure the relevant staff are familiar with this QRG, that it is implemented according to the guidelines as outlined within, and that there is compliance by all staff members.
Guideline Details
What does this look like in practice?
- Skin & risk assessment on arrival to department.
- Regular pressure area care.
- Monitor nutrition and fluid intake.
- ACE review.
- Promote independence.
- Regular toilet routine.
- Air mattress & pressure relieving devices.
- Manage existing pressure Injuries with best practice guidelines.
- Wound charts & wound dressings.
- Encourage patients to participate in the care of preventing pressure injuries.
- Riskman incident reporting on pressure injuries.
- Inform patients & families of risks, prevention strategies & management of pressure injuries.
All patients who present to the Emergency department regardless of age will require a skin integrity & mobility assessments to be undertaken. Helping identify at risk patients on admission.
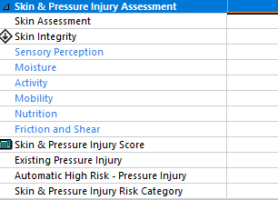
Figure 1: Risk screening for skin integrity
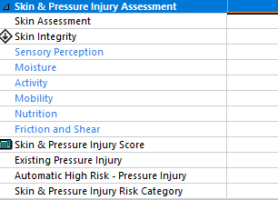
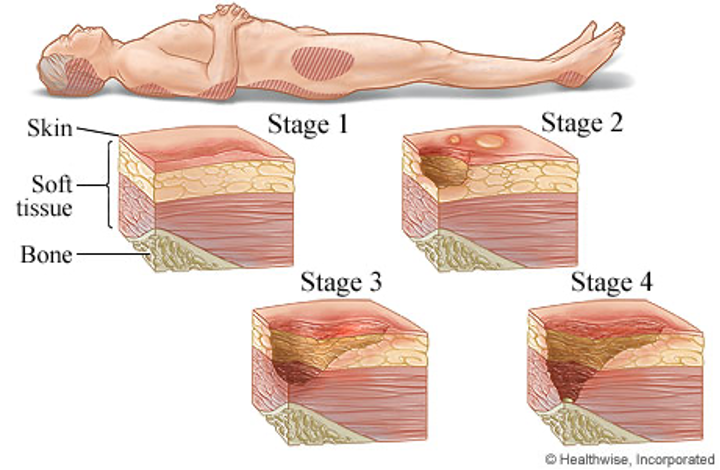
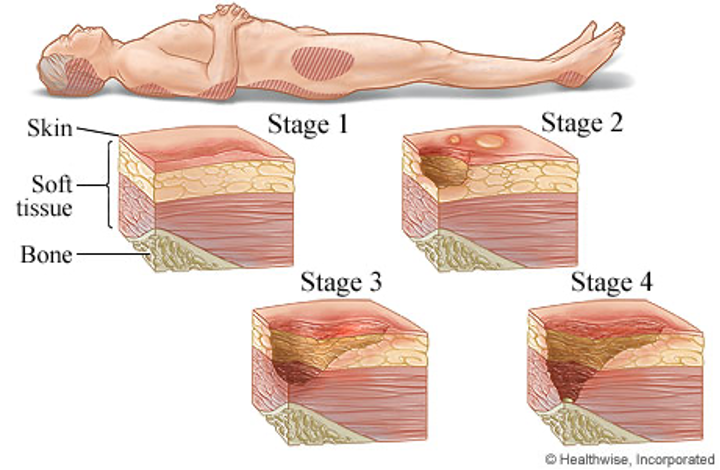
Figure 2: Pressure injury stages
Important to know
- Pressure injuries increase the risk of hospital-based complications.
- Associated with increased morbidity & mortality.
- Associated with increased pain, loss of mobility & independence.
- Most pressure injuries are preventable.
Best practice includes
- Vigilant screening.
- Comprehensive assessment.
- Implementing pressure injury prevention strategies.
- Evaluating effectiveness of pressure injury prevention strategies.
- Engaging patients in their own pressure injury prevention.
Risk Factors for pressure injuries
- Impaired mobility, sensory perception & activity.
- Any reduction in the patient’s ability to change their own position.
- Neurological conditions, spinal cord injuries, trauma, obesity, diabetes.
- Medications.
- Moisture, shear & friction.
- Nutrition.
- Demographics.
- Oxygen delivery.
- Skin temperature.
- Chronic illness.
The ability of the skin to tolerance pressure can be influenced by friction & shear, moisture, ageing, nutrition, hydration & chronic illnesses.
What should I include in my skin assessment?
Head to toe assessment looking at the integrity of the skin, temperature, colour, skin turgor, moisture, areas of pain & pressure damage from lines & devices.
Pay close attention to bony prominences such as heels & sacrum. Looking for erythema, blanching, localise heat, oedema & skin breakdown. Considering assessment of mobility, activity, recent weight loss, continence, cognitive function, nutrition & other external factors.
Strategies
- Regular repositioning.
- Pressure relieving devices.
- Promote independence with mobility.
- Continence aids.
- Ensure patient’s skin is dry.
- Avoid trauma from devices.
- Optimise hydration & nutrition.
- Document skin assessment & pressure injuries.
- Communicate with patient & carers.
Supporting Documents
Document Governance
| Title: |
Skin Assessment and Preventing Pressure Injuries |
| Version: |
1.0 |
| Date Published: |
February, 2021 |
| Date of scheduled review: |
August 2024 |
| Author: ED Leadership Team |
Approver: ED Leadership Team |
| Reviewed By: Ian Law |
Date: August 2023 |