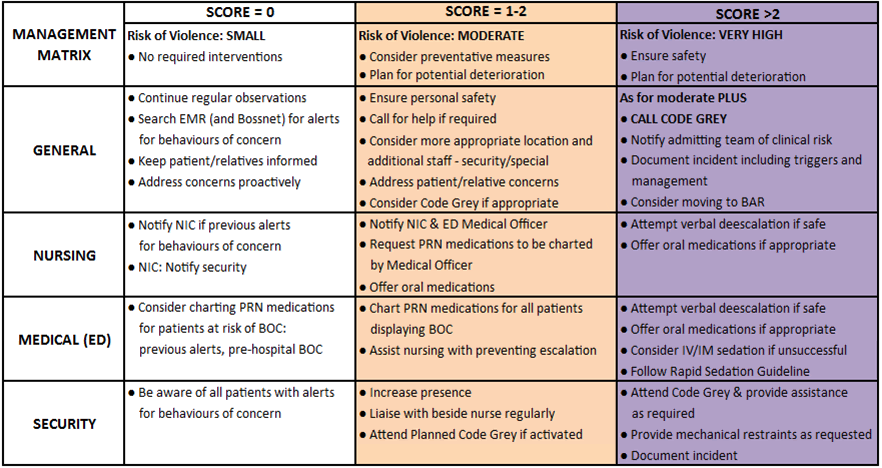
The Management Matrix collocated with the “BOC Chart” should guide all management
Non-pharmacological management:
- De-escalation
- Reducing environmental triggers
- Physical and mechanical restraint
- Additional staffing e.g. specials
Pharmacological management
According to the Pharmacological Management of Acute Behavioural Disturbance in the Emergency Department Guideline (Emergency Department DG-GC6)
Behaviour Assessment Unit (BAU; SHED specific)
The operational and functional purpose of BAU is to manage and assist patients that present at high risk of self-harm or causing harm to others, including highly agitated and/or aggressive patients.
The BAU provides a dedicated space within which a multidisciplinary team can work. The environment is designed to be low stimuli and have increased privacy, improving the patient experience.
BAU will operate 24/7, 365 days. It will be staffed with nursing, medical and mental health clinicians.
Behaviour Assessment Room (BAR)
The purpose of using the BAR is to provide a safe environment to manage behaviours of concern in a location which maintains privacy for the patient, and limits distress for other patients and relatives. There are two BARs that form part of the overall BAU with nursing and medical support.
The decision to utilise the BAR is made by the Senior Medical Officer, in collaboration with the Nurse in Charge and Team Leader of Resus/BAU of the shift and where appropriate, in consultation with specialist services (e.g. Mental Health clinicians and security).
This decision will be based on the risk of violence, considering the following:
-
- Absolute indication:
- BOC score >2;
- Arrival with police escort under Section-351 of the Mental Health Act.
- Relative indications as deemed necessary:
- BOC score 1-2;
- Arrival with ambulance with pre-notification of behaviours of concern.
The use of this space is outlined in more detail in DP-EP4 Prevention and Management of Behaviours of Concern in the Emergency Department (Including use of Behavioural Assessment Rooms)
Security responses
Security are in attendance in ED 24 hours a day and should be proactively engaged through:
- Planned Code Grays (BOC Call)
- Unplanned Code Grays
- Duress activation
- Code Blacks