This document is a summarised version of OP-GC2-Preventing Patient Falls and Harm from Falls Procedure. The summary has been created to be Emergency Department specific, and has been endorsed by the ED Leadership Team. Staff should review the PPG if they require further information.
Overview
This QRG aims to provide staff with an overview of the management and prevention of falls within the Emergency Department. Every patient is at risk of a fall during their stay, therefore all patients should be screened on admission. The falls risk assessment should be completed in the Nursing initial assessment section of FirstNet.
Applicability
This QRG applies to all presentations to the Emergency Department.
Responsibility
It is the responsibility of the Nurse Unit Managers and Directors of the Emergency Departments of each site to ensure the relevant staff are familiar with this QRG, that it is implemented according to the guidelines as outlined within, and that there is compliance by all staff members.
Guideline Details
What does this look like in practice
Reasons leading to a fall
- The type or amount of medications a patient is receiving.
- Environment.
- Toilet access.
- Available equipment.
- Medical conditions.
- Personal factors.
- Reduced eye sight
- Loss of balance.
- Weaker muscles & stiffer joints.
- Fall within the last 12 months.
- Mental state.
- Admission to hospital with a fall.
- Require assistance & supervision to mobilise & transfer.
- Agitated, confused or disoriented.
Risk assessment
On arrival to the emergency department each patient requires the completion of the risk screening tools on the back of the nursing chart to be completed. This includes the following questions to be asked. The falls risk assessment section of the Adult Observation Chart is included in Figure 1.
Figure 1: Falls risk assessment section of the Adult Emergency Department Observations Chart

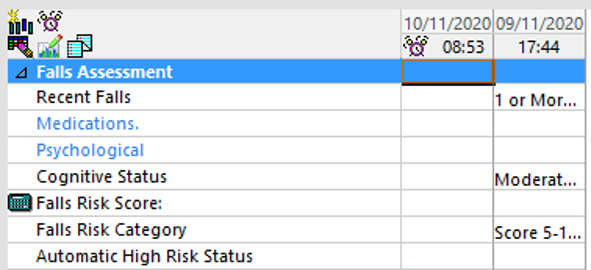
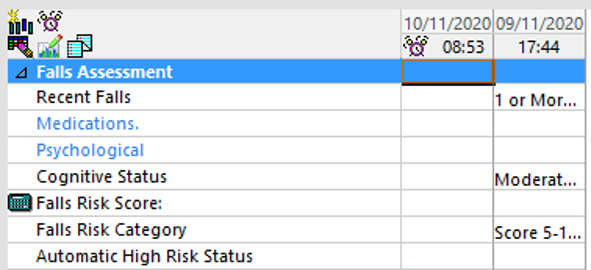
Once completed undertake the daily falls risk assessment on EMR (Figure 2). This is also to be completed if a fall occurs or if there is a change in the patient’s mobility or medical condition.
Figure 2: EMR Daily Falls Risk Assessment
Maintaining a safe environment for all patients
- Ensuring the Emergency trolley is lowered to the ground.
- Introduce self to the patient & orientate to new surroundings.
- Ensure brakes are on the trolley.
- Ensure patient wears suitable footwear.
- Hand patient the call bell & explain how to use it.
- Keep curtains open to visualise all high-risk patients.
- Ensure appropriate cubicle lighting.
- Keep lights on to assist with vision.
- Remove all unnecessary items from cubical.
- Attend to regular vital signs.
- Implement a regular toileting regime.
- Assist those who require help to the toilet & shower.
- Place items such as walking aids, water, call bell & glasses within reach.
- Place patients close to the nursing station if clinically appropriate.
- Escalate to NIC if patient is a falls risk to prioritise timely inpatient admission if needed.
Educating patients & carers
- Take the time to orientate patient & carers, pointing out key areas such as the toilet & call bell.
- Inform of high traffic areas, wet floors, swinging doors & where hand rails are available.
- Assertion what walking aids are used & how the patient mobilises.
Management
- Implement all standard safety measures regardless of the patients falls risk.
- Use clinical judgement.
- Place falls signs outside of patients cubical.
- Take falls history including strategies adopted in the home environment.
- Urinalysis.
- Bedside commode or bottle at night.
- Continence aids as appropriate.
- Bladder scan.
- Supervise mobility.
- Refer to ACE team.
- Lying and standing Blood pressures.
- During clinical handover inform of falls history & current management.
Post falls procedure
- Attend to full head to toe assessment & vital signs including neurological observations.
- Notify treating nursing, medical.
- Notify patient’s NOK.
- Conduct post fall huddle and document outcome in EMR
- Riskman & document incident in EMR
- Follow the actions in Table 1.
Table 1: Post patient fall clinical follow up
| Unwitnessed fall and possible head strike with anticoagulation therapy |
Unwitnessed fall and/or head strike without anticoagulation therapy |
Witnessed falls with no head strike |
- Patient is reviewed by medical officer
- Record vital and neurological vital signs (BP, HR, RR, O2, saturations):
- ½ hourly for 4 hours
- Then 2 hourly for 8 hours
- Then 4 hourly for 12 hours.
- Observe for change in level of consciousness, headache, vomiting, confusion and pupil size
- Escalate to an urgent clinical review or met call if patient deteriorates
|
- Record vital signs and neurological observations (BP, HR,RR, O2 saturations) ½ hourly for 4 hours, the 4 hourly for 20 hours
- Observe for change in level of consciousness, headache, vomiting and confusion
- Contact medical staff for review, to occur within 2 hours
|
- Record vital signs record vital signs and neurological observations (BP, HR,RR, O2 saturations) ½ hourly for 4 hours, the 4 hourly for 20 hours
- Contact Medical Staff for review within 4 hours
|
Supporting Documents
1. OP-GC2-Preventing Patient Falls and Harm from Falls Procedure
Document Governance
| Title: |
Managing and Reducing Falls in our Emergency Departments |
| Version: |
2.0 |
| Date Published: |
01/08/2021 |
| Date of scheduled review: |
March 2023 |
| Author: ED Leadership Team |
Approver: ED Leadership Team |
| Reviewed By: Ian Law |
Date: March 2023 |