February 14, 2021
Overview
This Theme of the Week, focuses on best practice processes for documenting in the EMR .
Alignment to Western Health Best Care Framework:
Safe Care & Coordinated Care
Why is this important:
Accurate and complete EMR documentation communicates to inpatient teams important information about the patient and the care they have received while in the Emergency Department. It also electronically documents care and clinical activity that may be useful in future admissions.
What does this look like in practice?
- Confirming patients details are correct.
- Recording & checking alerts and allergies.
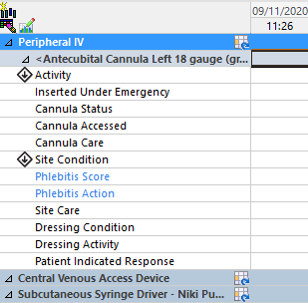
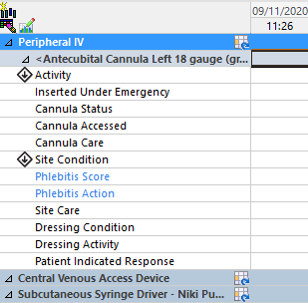
- Documenting lines & devices.
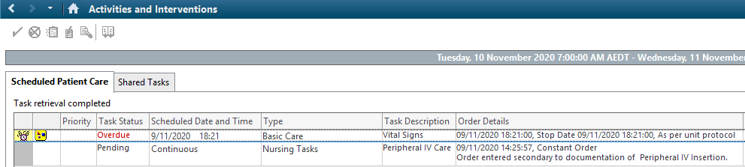
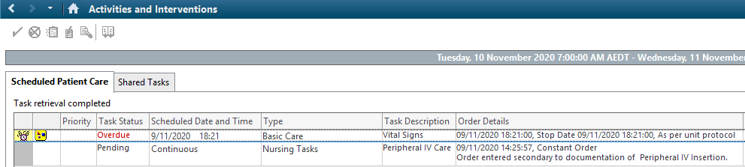
- Signing off requests under activities & interventions.
- Correctly filling out the MAR & documenting withheld medications.
- Correctly filling out the fluid balance chart.
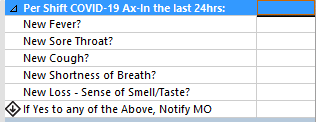
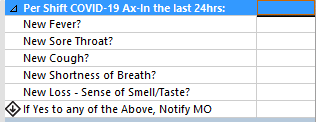
- Covid risk assessment.
- Document vitals for patient transfer to ward if needed.
EMR Tool
|
What it looks like:
|
Shift- commencement and pre-transfer COVID screen
|
 |
Peripheral IV Management
|
 |
EMR Clinical Tasks
|
 |
Performance
MAR audits.
Intravenous Cannula Audits.
QRGs:
Electronic Medical Records Documentation Quick Reference Guide