This document is a summarised version of OP-GC2-Comprehensive Care, OP-GC2-Preventing Patient Falls and Harm from Falls Procedure, OP-GC5-Advance Care Planning and End of Life Care, OG-GC2-Delirium Guidelines, OP-GC2-Pressure Injury Prevention and Management, The summary has been created to combine best practice information into one document specific to the Emergency Department, and has been endorsed by the ED Leadership Team. Staff should review the PPGs if they require further information.
Overview
This QRG aims to provide staff with an overview of risk screening within the Emergency Department. Risk screening in ED supports the Comprehensive Care Standard to identify patient needs and prevent harm. It includes actions related to falls, pressure injuries, mental health, cognitive impairment and end-of-life care.
Applicability
This QRG applies to all presentations to the Emergency Department.
Responsibility
It is the responsibility of the Nurse Unit Managers and Directors of the Emergency Departments of each site to ensure the relevant staff are familiar with this QRG, that it is implemented according to the guidelines as outlined within, and that there is compliance by all staff members.
Guideline Details
What does this look like in practice?
Risk assessments
On arrival to the emergency department place patient in a hospital gown for assessment and complete the risk assessments in the Nursing Initial assessment section of FirstNet.
If the answer to any of the risk screening questions is yes – the appropriate strategies should be implemented as soon as practicable.
End of Life Care:
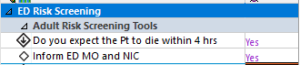
- Complete the End of Life Care screening tool (Figure 1)
Figure 1: End of Life screening tool.
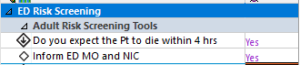
If answer is yes:
Mental Health
- Complete Mental Health screening tool (Figure 2)
Figure 2: Mental Health screening tool
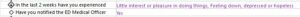
If answer is yes to any:
- Refer to ED Medical Officer
- If required, patient can be referred to EMH/ECATT by ED Medical Officer
- Please refer to the Patient Streaming – SHED QRG for further information regarding streaming of patients with mental health care needs at SHED
- Please refer to MHAOD Care in Emergency Departments QRG for further information
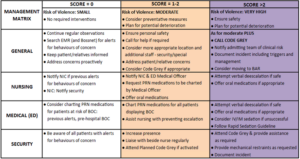
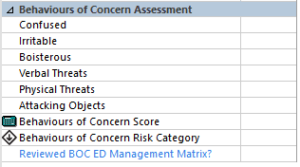
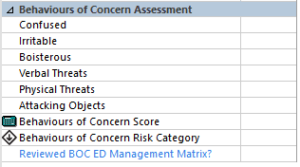
Behaviours of Concern Risk screening
Risk for behaviours of concern (BOC) should be assessed at minimum:
- Hourly in Adult Acute Area, Resuscitation Area, The Hub and BAU/BAR and with all vital signs assessment
- Two hourly in Short Stay Unit and with all vital signs assessment
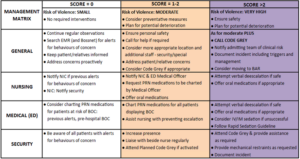
Risk should be assessed against the BOC Management Matrix with appropriate interventions guided by the matrix as outlined in Figure 3.
Figure 3: Behaviours of Concern Observations and Management Matrix
|
  |
Delirium
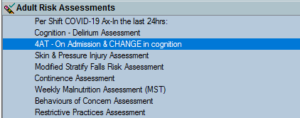
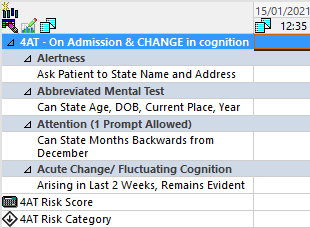
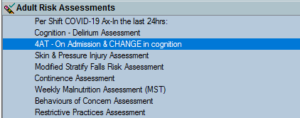
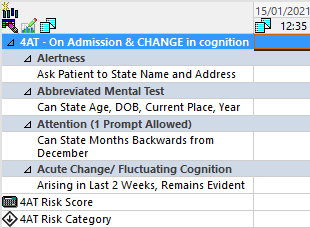
Complete 4AT on EMR (Figure 5.1 & 5.2)
|
|
Figure 5.1 EMR Adult risk assessments
|
 |
|
|
Figure 5.2 EMR 4AT
|
 |
Pressure Injuries and Falls Risk
Skin Assessment and Preventing Pressure Injuries – Western Health Emergency Department (wh.org.au)
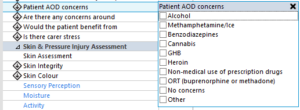
Alcohol and Other Drugs
Complete the Alcohol and Other Drugs screening tool
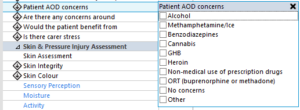
If answer is yes to any:
- Refer to AOD clinician
- If AOD clinician unavailable, consider referral to ACE or treating medical officer
- Consider commencing Alcohol Withdrawal Scale (AWS)
- Please refer to MHAOD Care in Emergency Departments QRG for further information
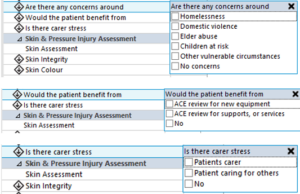
Advice, Coordination and Expertise:
- Complete the Advice, Coordination and Expertise (ACE) risk screening tool (Figure 8)
ACE risk screening tool.
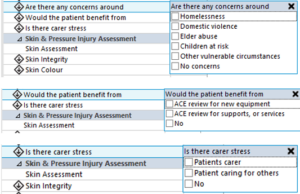
If answer is yes to any:
- Refer to ACE
- If after hours or ACE unavailable, considering referral for follow up phone call at home or Short Stay Admission for inpatient ACE review
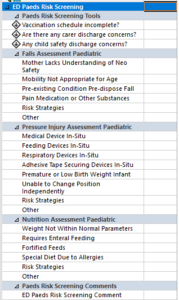
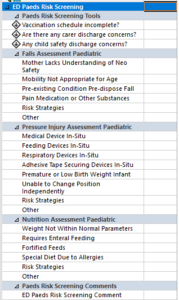
Paediatric Considerations
Risk Assessment: FirstNet Nursing Initial Assessment
Full skin check should be completed at initial presentation for patients under 3 years old and for patients assessed as at risk of pressure injury. This may need to be supported by the presence of a parent or guardian.
Specific consideration should be given to the securement of medical devices including IVC and NGT as these devices present a risk of pressure injuries developing.
Areas at risk of pressure injury should be checked minimum of hourly, and more frequently where deemed appropriate by clinical staff.
If pressure injury is found,
- notify treating medical officer and NIC
- Consider repositioning of medical device or replacement if required
- Implement pressure relieving interventions
- Complete Riskman
Falls Risk
- Implement appropriate strategies
- Notify nurse in charge if higher visibility cubicle required
- Support and encourage parent’s constant presence if suitable
- Place cot sides up and bed in lowest possible position to the ground
Supporting Documents
Document Governance
| Title: |
Risk Screening in the Emergency Departments |
| Version: |
2.0 |
| Date Published: |
May, 2022 |
| Date of scheduled review: |
February 2024 |
| Author: ED Leadership Team |
Approved: ED Leadership Team |
| Reviewed By: Ian Law |
Date: February 2023 |